This qualitative study – a joint study between our Pharmacy Department and the School of Pharmacy, University College Cork (UCC) - highlights the need for more tailored guidance in managing weight gain caused by antipsychotic medications.
Published in BJPsych Open in 2024, the research explores gaps between current clinical guidelines and the needs of patients, taking on patient experiences and preferences in relation to antipsychotic-induced weight gain management guidance in clinical practice.
The challenge of antipsychotic-induced weight gain
Clinically significant weight gain—defined as a 7% increase in body weight compared to baseline—has been linked to almost all antipsychotic medications. This weight gain tends to occur largely independent of dose and, among susceptible individuals, typically accumulates quickly within weeks of starting treatment. However, the extent of weight change varies widely, even among those prescribed the same medication, with some people experiencing minimal changes, while others gain significant amounts of weight.
To protect the physical health of people living with a mental health difficulty and prescribed an antipsychotic, managing weight gain proactively and effectively is of crucial. One barrier for clinicians is the lack of comprehensive, evidence-based guidance to inform their practice. Current recommendations primarily focus on general population weight management strategies, such as self-led lifestyle changes, while pharmacological interventions, such as the use of medications to counteract increased appetite, are generally considered only when other options have failed.
Current guidelines and limitations
While limited international guidelines exist, their development has largely been informed by expert opinion, rather than the lived experiences of those directly affected. Current guidance often applies a uniform approach that does not fully consider the unique challenges of antipsychotic-induced weight gain, which differs in both its causes and its management from other forms of weight gain.
Participants in this study expressed that current guidelines are overly simplistic, lacking the specificity and scope required to address the diverse needs of individuals affected by this side effect.
Listening to patient experiences
This study is the first to explore the management preferences of patients with experience of managing weight gain from antipsychotics and to compare this with current management algorithms informing clinicians’ practice. A diverse range of 17 individuals with experiences of mild to severe antipsychotic-induced weight gain and mental health difficulties, including schizophrenia, bipolar affective disorder and major depressive disorder, were interviewed regarding:
- their experiences of managing antipsychotic-induced weight gain
- the acceptability, feasibility, and transferability of current management algorithms and the interventions contained within (both pharmacological and non-pharmacological)
- how patient-centred care can be better integrated into Irish healthcare settings.
The need for more individualised guidance
Participants in this study reported that current guidance is over-simplified, lacks the specificity and scope required and endorses a homogenous management approach to an extensively heterogenous side effect, both in presentation and manageability, including response to intervention. Participants provided experiences of appetite increases secondary to antipsychotic treatment.
One participant said: “It’s a hunger you just can’t do anything about, you know, food doesn’t satisfy it. I couldn’t any other way than be hungry. I could eat twice the amount of dinner and you’re still as hungry as when you started.”
While perhaps pragmatic, beyond minor weight increases, participants reported that behavioural changes alone were insufficient to manage antipsychotic-induced weight gain. Continued clinician recommendations to implement self-led lifestyle changes could worsen sense of isolation, internalised stigma, and reduce the likelihood of seeking further help.
A participant explained: “…it leaves me feeling kind of isolated as well because how it looks is that I am not making an effort to improve my position and then I don’t want to see people and be judged for it…being overweight and having mental health issues, I just don't want to be perceived as lazy.”
Rethinking treatment approaches
Disagreement with the recommendation of behavioural changes as a uniform, first-line strategy was particularly evident among participants who were severely unwell when they initiated antipsychotic treatment. Many viewed pharmacological adjuncts, such as metformin, as relevant and acceptable interventions and suggested that these be offered earlier than current guidelines endorse.
A participant described: “If you were dealing with psychosis, if somebody has been very ill, they may not be able to make diet and lifestyle changes. In their case the tailoring may involve more preventative use of metformin because they just may not be in that position to make those decisions for themselves that really require being very proactive at a time when you are recovering.”
Participants also suggested that preventive measures, such as prescribing medications to counteract weight gain at the start of antipsychotic treatment, should be considered.
For one participant: “That would be like if you had cancer, the chemotherapy or radiation or whatever is making you sick, there is immediately an anti-sickness drug…it’s not something you wait to be told about.”
Recommendations for improved guidelines
Findings from this study indicate a strong need for changes in antipsychotic-induced weight gain management guidance to improve its applicability and transferability across different individuals and contexts. Participants described patient-centred weight management as being proactive, individualised, holistic, and collaborative.
Ways in which these four tenets of patient-centred management can be enacted in management guidance and within psychiatric services is outlined in the image below.
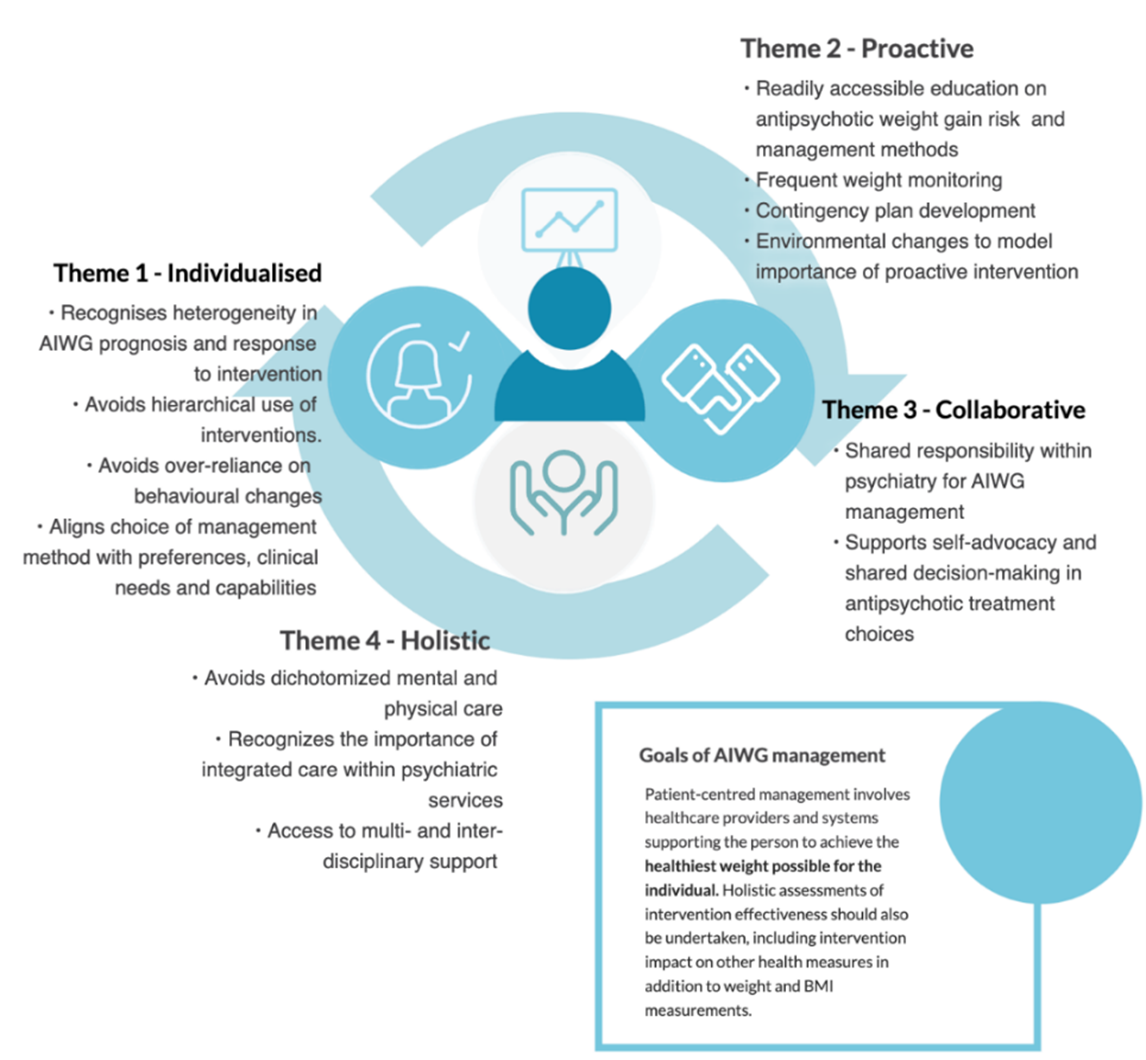
Participants emphasised that antipsychotic-induced weight gain is a unique cause of weight gain, often in unique contextual circumstances, and requires an equally distinctive approach to management. Improved recommendations in antipsychotic-induced weight gain management recognise diversity amongst individuals in the initial risk and subsequent trajectory of antipsychotic-induced weight gain and allow for intervention use to be tailored towards risk of overweight or obesity, individual physical and mental health capabilities, and their treatment preferences.
The full study is available in BJPsych Open for further reading.





